Measles in 2025: A Comprehensive Overview
Measles virus (Morbillivirus abbreviated as MV, but more recently MeV) is the causal agent of measles disease, thought to have existed at least 4,000 years ago, affecting predominantly infants, but also immunocompromised individuals remaining a public health issue today globally. In this review, we discuss the historical background about MeV infection to modern-day research on measles disease, current epidemiology, but also what is known about immunisation against it. We report what is known about the viral structure and the function of the viral proteins. This additionally covers the cellular structure of MeV, mechanisms, and clinical aspects of infection. Including a review of topics like cellular receptor-associated entry factors, to the immunology of MeV infection. In this review, the current knowledge of innate immune responses during infection is explained, which involves changes to chemokine and cytokine expression, finalised by the present understanding of adaptive immune responses to MeV. The genomic stability of the MeV proteins is explained and suggestive that it could be the third Image Credit: pathogen with eradication potential (after the variola and rinderpest viruses). Further biological and immunological clarification as to how this could occur is explained here:
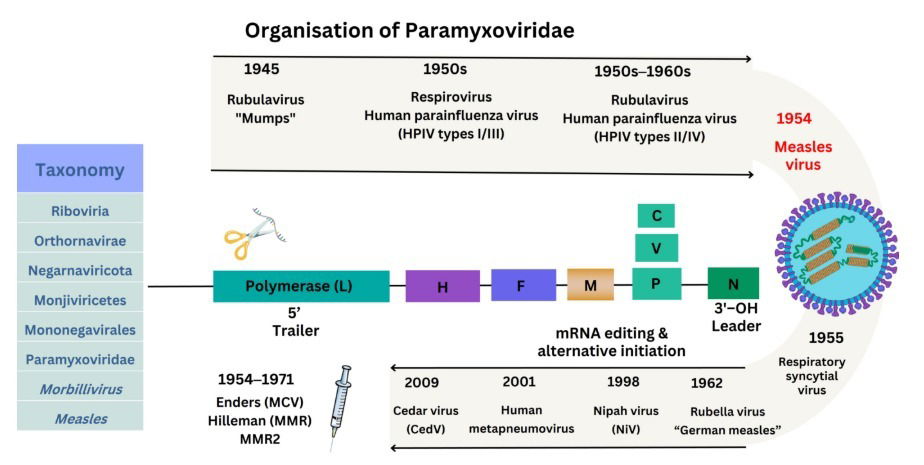
Image Credit: Brent Brown: Understanding measles virus: from isolation to immunological cellular mechanisms and immunisation 1954–2024
Measles in 2025: A Comprehensive Overview
Measles is a highly contagious viral disease that remains a significant global health challenge despite the availability of a safe and effective vaccine. This article provides a comprehensive overview of the state of measles as of the year 2025, reflecting on the latest trends, outbreak controls, vaccination strategies, and anticipated challenges in the fight against this persistent disease.
Introduction
Despite advancements in public health, measles continues to be a considerable concern worldwide, particularly in low and middle-income countries with insufficient health infrastructure. The discussion that follows offers insights into the key aspects of measles control and eradication efforts as of 2025.
1. Global Epidemiology of Measles
- The incidence of measles globally has seen fluctuations, with significant outbreaks occurring in regions with low vaccination coverage. As of 2025, there are approximately 120,000 reported cases annually, a statistic that shows a decrease compared to the previous decade. However, sporadic outbreaks highlight the ongoing challenges of achieving global immunity.
- Population movements, including mass migration and displacement due to conflicts and natural disasters, continue to complicate measles control. These movements often lead to vaccination gaps and increased susceptibility to outbreaks.
- Countries with robust health systems have managed to maintain high vaccination coverage; however, vaccine hesitancy remains a significant issue, with misinformation and distrust in vaccines leading to lower uptake rates in certain regions.
- In 2025, as of April 17, 2025, a total of 800 confirmed* measles cases were reported by 25 jurisdictions in the USA: Alaska, Arkansas, California, Colorado, Florida, Georgia, Hawaii, Indiana, Kansas, Kentucky, Maryland, Michigan, Minnesota, New Jersey, New Mexico, New York City, New York State, Ohio, Oklahoma, Pennsylvania, Rhode Island, Tennessee, Texas, Vermont, and Washington. 3 or more fatalities have been reported this year with 1 under investigation. Source:
- In 2025, the ECDC reported an annual total of 28 791 cases of measles until February 2025. Of the 28 791 cases with known age, 12 816 (44.5%) were in children under five years of age; and 7 880 (27.4%) cases were aged 15 years or older. The highest notification rates were observed in infants under one year of age (928.4 cases per million) and children aged 1-4 years (542.6 cases per million). Of 26 669 cases (100.0% of all cases) with a known age and vaccination status, 22 992 (86.2%) were unvaccinated, 2 378 (8.9%) were vaccinated with one dose of a measles-containing vaccine, 1 213 (4.5%) were vaccinated with two or more doses, and 50 (0.2%) were vaccinated with an unknown number of doses. Fourteen deaths attributable to measles were reported to ECDC during the 12-month period. See report.
- In 2025, the UK reported a total to date of 213 cases as of 21st April 2025 from the UK Health Security Agency
2. Advances in Vaccine Strategies
- The development of combined vaccines that address multiple diseases, including measles, mumps, rubella, and varicella (MMRV), continues to improve. These vaccines offer the benefit of reducing the number of shots required, thereby improving compliance and coverage rates.
- New delivery methods for vaccines, such as needle-free systems, are under development. These technologies aim to increase vaccine acceptance and reach populations in remote areas where healthcare services are limited.
- Targeted vaccination campaigns in high-risk areas have been ramped up, using data-driven approaches to identify and immunize children who missed routine vaccinations during the global upheavals caused by the COVID-19 pandemic.
3. Public Health Policies and Government Role
- Governments around the world are intensifying efforts to integrate measles vaccination into national immunization programs. This integration often includes mandates or incentives for vaccination, particularly in school-aged children.
- Funding for measles vaccination programs has increased, with international organizations such as the World Health Organization (WHO) and GAVI, the Vaccine Alliance, playing pivotal roles in supporting low-income countries.
- There is a push towards the elimination of measles, with global health leaders setting ambitious goals for eradicating the disease by 2030. Achieving this goal requires sustained commitment and resources, particularly in regions where healthcare infrastructure needs strengthening.
4. Technological Innovations
- The use of geographic information systems (GIS) and other digital tools has been instrumental in planning and implementing vaccination campaigns more effectively. These tools help in pinpointing outbreak hotspots and understanding vaccination coverage gaps.
- Artificial intelligence (AI) and machine learning are being leveraged to predict outbreaks and model scenarios for intervention strategies, providing a proactive approach to managing measles risks.
- Blockchain technology has begun to find applications in vaccine distribution, ensuring the integrity of vaccine supply chains and helping to prevent counterfeiting of vaccines, which is crucial in maintaining public trust and safety.
5. Challenges and Barriers to Eradication
- While there has been significant progress, measles eradication faces challenges such as vaccine hesitancy, logistical barriers in vaccine delivery, especially in war-torn regions, and the resurgence of diseases following natural disasters.
- Financial constraints in low-income countries hinder sustained immunization efforts, necessitating continuous financial support from the international community.
- The variation in measles vaccine laws and policies globally affects the standardization of vaccination efforts, requiring a more harmonized approach to achieve global immunity.
6. Public Awareness and Misinformation
- Continued efforts are necessary to combat misinformation about vaccines. Educational campaigns and partnerships with local influencers and community leaders have proven effective in this regard.
- Social media platforms and other online communities play a pivotal role in spreading factual information as well as misinformation, making it crucial for health authorities to engage actively with these platforms to provide reliable data about measles and its prevention.
- Special attention is given to training healthcare providers not just in high-income areas but globally, ensuring they are equipped to provide accurate information and respond to vaccine hesitancy effectively.
Conclusion
Looking ahead to the rest of the decade, the global health community remains optimistic about the potential to reduce, and eventually eliminate, measles. However, this goal requires ongoing vigilance, adaptation to new challenges, and sustained cooperation among nations, healthcare providers, and the public. The lessons learned from the COVID-19 pandemic about the fragility and interconnectedness of global health will undoubtedly influence measles eradication efforts moving forward.
In conclusion, whilst significant challenges remain, the strategies, innovations, and commitments outlined will be critical in shaping the future landscape of measles control and eradication into 2030 and beyond reviewed in this manuscript.